What is Diabetes?
Diabetes (also known as Diabetes Mellitus) is a lifelong metabolic condition where the body either resists insulin’s effects or fails to produce enough insulin, leading to glucose buildup. This can result in severe health complications like heart disease, kidney failure, blindness, and limb amputations.
Types of Diabetes
- Type 1 Diabetes:
- It typically develops in childhood and is currently not preventable
- Caused by the immune system attacking insulin-producing pancreatic cells, leading to insulin deficiency.
- Requires daily insulin administration.
- Type 2 Diabetes:
- Results from insufficient insulin production or ineffective insulin use.
- Caused by genetic and environmental factors but can be entirely prevented if diagnosed early.
- Symptoms are often milder or absent compared to Type 1 diabetes.
The Global Diabetes Crisis
The number of people with diabetes increased dramatically from 200 million in 1990 to almost 830 million in 2022, signalling a global health crisis that demands urgent action. This rise, particularly in Type 2 diabetes cases, is strongly linked to obesity and reduced physical activity.[1]
Key Challenges
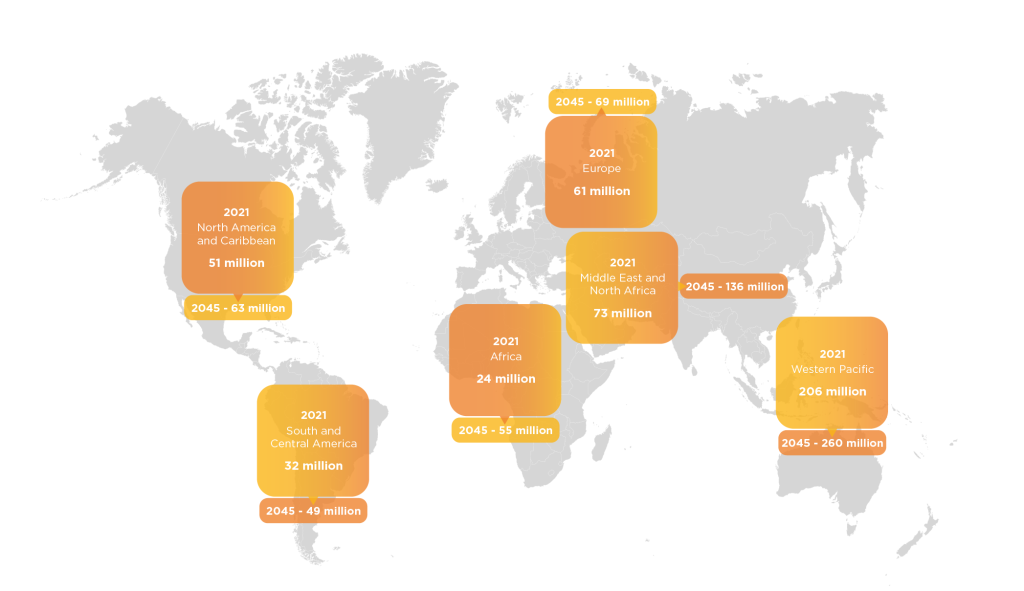
Global Diabetes Prevalence and Growth from 2021-2045
The map below demonstrates the estimated global number of diabetes cases found in people from the ages of 20-79 years old in 2021 and the projected growth in each region up to 2045.
537 million adults (20-79 years) are living with diabetes – 1 in 10. This number is predicted to rise to 643 million by 2030 and 783 million by 2045.[4]

Diabetes Symptoms and Complications
Short-Term Complications
- Hypoglycemia: Low blood glucose (<4 mmol/L) caused by missed meals, excessive insulin, or other factors. Symptoms: fatigue, hunger, anxiety, confusion, and in severe cases, unconsciousness.[5]
- Diabetic Ketoacidosis (DKA): Often an initial indicator of diabetes, triggered by insufficient insulin, leading to fat metabolism and ketone production. Symptoms: dry mouth, thirst, frequent urination, high blood glucose (>300 mg/dL), and ketones in urine.[6]
- Hyperosmolar Hyperglycemic State (HHS): Extremely high blood glucose (>40 mmol/L) caused by ineffective medication or illness. Symptoms: thirst, nausea, dry skin, disorientation, and gradual loss of consciousness.[7]
General Diabetes Symptoms
Frequent urination (especially at night), persistent thirst, fatigue, blurred vision, weight loss, genital itching, and slow-healing wounds.
Long-Term Complications
- Cardiovascular Disease (CVD): Chronic high glucose damages blood vessels, increasing risks of heart disease and stroke, especially with smoking or inactivity.
- Retinopathy: Damage to retinal blood vessels due to high glucose, potentially leading to blindness.
- Neuropathy: Nerve damage from poor nutrient delivery. Types include sensory (tingling/numbness), autonomic, and motor neuropathy. Sensory damage can lead to unnoticed injuries, infections, and amputations.
- Nephropathy: Prolonged high glucose harms kidney function, potentially leading to kidney failure and dialysis.
HbA1c Testing for Diabetes Diagnosis
What is HbA1c?
HbA1c refers to glycated hemoglobin, a protein in red blood cells that binds irreversibly with glucose. Since red blood cells live for 8–12 weeks, measuring HbA1c provides an average blood glucose level over this time frame. Higher HbA1c levels indicate poorer blood sugar control, increasing the risk of diabetes-related complications.
Advantages of HbA1c Testing
- Provides an average glucose measure over 8–12 weeks, unaffected by recent food intake or patient compliance issues.
- No fasting or waiting period is required, making it a convenient and reliable diagnostic method.
Limitations of HbA1c Testing
HbA1c is unsuitable for certain situations, including:
- Children.
- Pregnancy.
- Symptoms of diabetes lasting less than two months.
- Suspected Type 1 diabetes.
- Acute pancreatic damage or surgery.
- Genetic, hematologic, or illness-related factors.
Comparison to Glucose Testing
Traditional glucose tests, such as fasting glucose or oral glucose tolerance tests (OGTT), rely heavily on patient compliance. For fasting glucose tests, patients must fast for at least eight hours, while OGTT requires patients to ingest a glucose drink and return for testing two hours later. Both methods are prone to inaccuracies due to noncompliance or improper test administration.
Understanding Ketosis and β-Hydroxybutyrate
What is Ketosis?
Ketosis occurs when the body lacks sufficient glucose for energy and begins metabolizing stored fats in the liver. This process produces ketones—acetone, acetoacetate, and Beta-Hydroxybutyrate (BHB). Normally, ketones are broken down by the body, but excessive buildup can result in ketoacidosis, a potentially fatal condition.
Importance of Monitoring Ketosis
Monitoring ketosis is critical in conditions like DKA, particularly in patients with Type 1 diabetes, where accelerated ketone production overwhelms the body’s ability to process them. Measuring ketones, particularly BHB, helps diagnose DKA, track treatment effectiveness, and confirm metabolic status alongside other tests like glucose and pH levels.
Methods for Testing Ketosis
- β-Hydroxybutyrate (BHB) Blood Testing:
- Reliable, quantitative, and provides precise monitoring of ketosis and ketoacidosis.
- Offers advantages such as earlier detection, faster treatment response, shorter hospital stays, and reduced lab tests.
- BHB levels are a stable and accurate indicator of metabolic status.
- Nitroprusside Urine Testing:
- Detects acetone and acetoacetate but cannot detect BHB.
- Provides only qualitative results, is prone to false positives and negatives, and is affected by fluid intake, urine concentration, and reagent stability.
- Less reliable compared to BHB blood testing.
β-Hydroxybutyrate is the most accurate and stable marker for monitoring ketosis and ketoacidosis. While urine testing is still common, blood-based BHB testing is superior for accurate diagnosis, therapy monitoring, and improved patient outcomes.
Summary
Diabetes is a global health crisis with rising cases and severe complications if unmanaged. Understanding its types, causes, and symptoms is key to prevention and treatment. Early diagnosis through reliable tests like HbA1c and proper disease management can reduce risks. Monitoring ketosis, especially with BHB blood testing, helps prevent life-threatening complications like diabetic ketoacidosis. By raising awareness, promoting early detection, and supporting better treatment, we can combat diabetes and improve health outcomes.
Sources:
[1] NCD Risk Factor Collaboration (NCD-RisC). (2023). Worldwide trends in diabetes prevalence and treatment from 1990 to 2022: A pooled analysis of 1,108 population-representative studies with 141 million participants. The Lancet – https://www.ifw-kiel.de
[2] NCD Risk Factor Collaboration (NCD-RisC). (2023). Worldwide trends in diabetes prevalence and treatment from 1990 to 2022: A pooled analysis of 1,108 population-representative studies with 141 million participants. The Lancet – https://www.ifw-kiel.de
[3] International Diabetes Federation. (2019). IDF Diabetes Atlas (9th ed.) – https://diabetesatlas.org
[4] International Diabetes Federation. (2021). Diabetes around the world in 2021: IDF Diabetes Atlas, 10th edition. International Diabetes Federation – https://diabetesatlas.org
[5] American Diabetes Association. (2009). Hyperglycemic crises in adult patients with diabetes. Diabetes Care, 32(7), 1335–1343. https://doi.org/10.2337/dc09-9032
[6] American Diabetes Association. (2009). Hyperglycemic crises in adult patients with diabetes. Diabetes Care, 32(7), 1335–1343. https://doi.org/10.2337/dc09-9032
[7]American Diabetes Association. (2009). Hyperglycemic crises in adult patients with diabetes. Diabetes Care, 32(7), 1335–1343. https://doi.org/10.2337/dc09-9032
NOTE: this guide is for information purposes only, and is not intended for use in patient diagnostics, screening, monitoring, or for making treatment decisions.